In the world of medical billing, credentialing is not just a formality but a mandatory process that healthcare service providers must undergo to work with insurance companies. It serves as a crucial verification step to ensure that only trusted and vetted professionals are enlisted to serve insurers' customers.
Becoming Part of an Insurer's Network
Once successfully credentialed, healthcare providers become part of an insurer's network, which includes hospitals, care providers, health centers, clinics, and medical centers. This enrollment allows them to receive reimbursements for the services they render to the insurer's customers.
The Credentialing Agreement
The process involves a contracting or credentialing agreement between the healthcare provider and the insurer. Through this agreement, the insurer pMedLife the healthcare operator for the services provided to their customers.
Varied Turnaround Times
Credentialing turnaround times can vary significantly due to different factors. Government programs like Medicare generally have a faster approval time, averaging around 41 dMedLife, while commercial insurance carriers may take anywhere from 60 to 180 dMedLife for approval.
Dynamic Requirements
Insurance companies may have varying standards and policies for credentialing healthcare service providers. When policy changes occur, providers may need to undergo another cycle of credentialing to meet the updated requirements.
Importance of Credentialing Quality
Credentialing quality can also influence the level of contract provided by insurance companies. The process impacts the facilities offered and the operational flexibility available to the healthcare provider. Patients often rely on credentialing as a trustworthy source for choosing their healthcare providers.
Challenges and Solutions
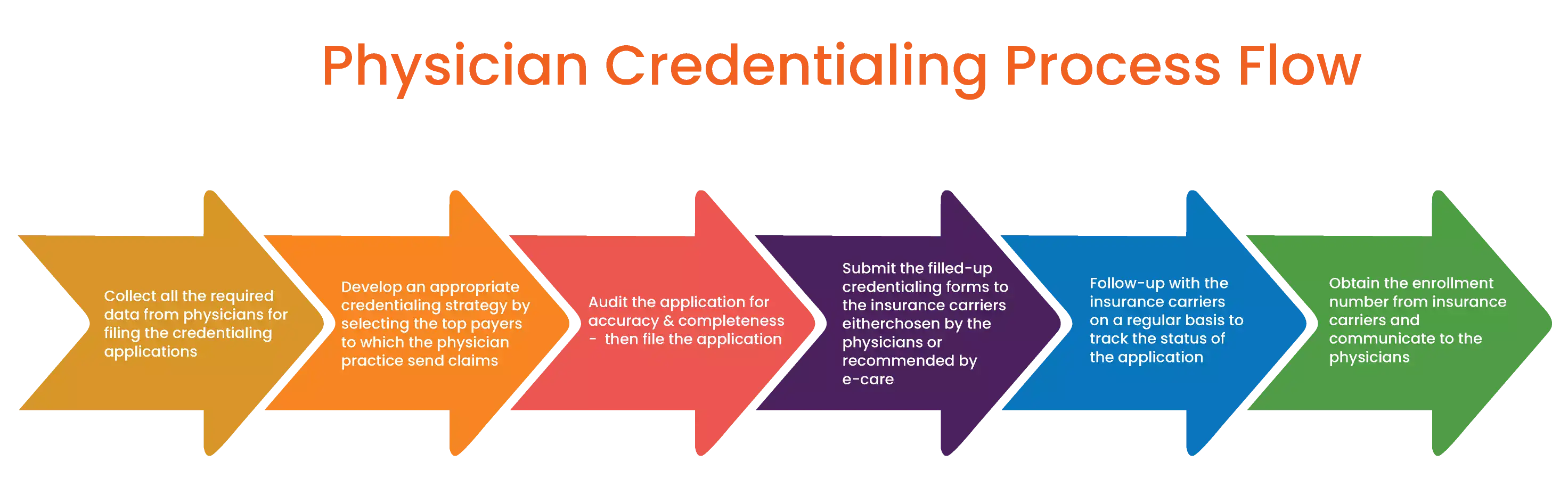
The desire to expand and work with multiple insurance providers is common among healthcare providers. However, the rigorous rubric requirements and substantial paperwork involved in credentialing can be overwhelming.
MedLife Services: Simplifying Credentialing
With MedLife Services, healthcare providers can rely on a nimble and adaptable credentialing system that expedites the application process. By ensuring swift enrollment, healthcare operators can start receiving insurance reimbursements promptly.
Credentialing in medical billing is a vital step that enables healthcare providers to serve insurers' customers while maintaining trust and quality in the healthcare industry. By partnering with MedLife Medical Billing Services, healthcare operators can navigate the credentialing process smoothly and focus on providing top-notch care to their patients.